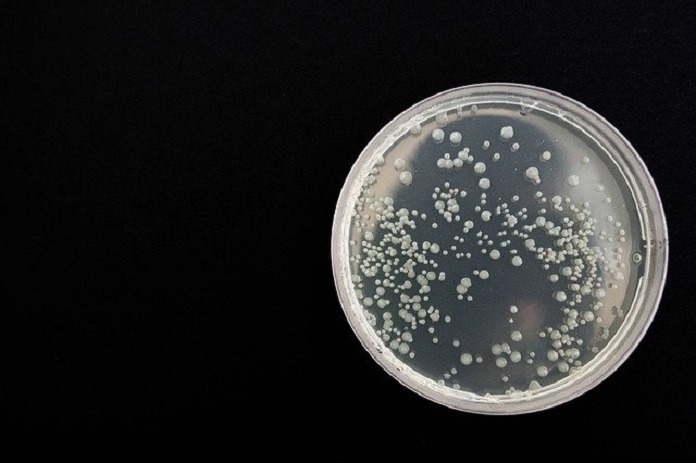
Candida parapsilosis is a fungus that can normally be found on both the human body and in nature. Under certain circumstances, it can also cause various diseases in humans that require medical treatment.
Candida parapsilosis is one of the approximately 611,000 different species of fungi. Within the 611,000 different species of fungi, only about 600 are able to cause infections in humans.1
Candida parapsilosis is a member of the Candida genus of fungi. It is one of the many endosymbionts of humans that can be classified as an opportunistic or facultative pathogen that can cause disease mainly in immune-compromised or susceptible hosts.1
It is also found in the environment and has been found in insects, soil, and marine environments.2
What leads to Candida parapsilosis infections?
Most Candida parapsilosis infections usually occur in the hospital and are associated with contaminated medical and prosthetic devices, catheters, fluids, and the hands of nurses and doctors.2
The main groups of people who are susceptible to these infections in the hospital include premature babies, patients needing gastrointestinal surgery, immuno-compromised patients (such as cancer patients), and those who may need extended use of a catheter.2
Other infections may result from injury and close contact with Candida parapsilosis (such as onychomycosis), or overuse of over-the-counter antifungal medications.2
What diseases are associated with Candida parapsilosis infections?
Generally, a fungal infection that is caused by a member of the Candida genus is referred to as candidiasis.1
While C. parapsilosis is an opportunistic pathogen, it has been associated with the following diseases/infections and can be contracted in hospital or healthcare settings or in other non-healthcare settings:
Fungemia
Fungemia is the presence of fungi or yeast in the blood, with the most common ‘form’ being candidemia (caused by members of the Candida genus). Fungemia caused by C. parapsilosis can result in ‘seeding’ of tissues leading to deeper infections. The mortality rate of C. parapsilosis fungemia can range from 4% to almost 45%.2
C. parapsilosis candidemia can be concerning in neonatal intensive care units (NICUs), as it is a major cause of the disease.2
Cardio endocarditis
Cardio endocarditis is inflammation of the heart valves, and currently fungal endocarditis accounts for one to six percent of the total cases.
Cases that are associated with C. parapsilosis include patients who have transcatheter aortic valve replacement, heart transplant, or who are receiving parenteral nutrition.3
Meningitis
Meningitis is inflammation of the central nervous system (specifically the protective membranes around the brain and spinal cord). While most people associate bacterial infections with meningitis, fungal infections can also cause meningitis. While C. parapsilosis is an infrequent cause of fungal meningitis, it can be the main cause of neonatal fungal meningitis.2
Peritonitis
Peritonitis is the inflammation of the peritoneum, or the membrane lining of the abdominal cavity and coverings of the abdominal organs. Fungal infections aren’t typically the cause of peritonitis. In fungal peritonitis, depending on the species, the mortality rate can be as high as 44%.2 For fungal peritonitis to occur, patients usually have undergone previous antibiotic treatment for bacterial peritonitis, or patients are doing continuous dialysis treatment for end-stage renal disease.2
Endophthalmitis
C. parapsilosis has been associated with invasive eye diseases—specifically endophthalmitis. This is an infection in the eye, which can follow cataract surgery or lens implantations.2
Arthritis
With a diagnosis of fungal arthritis (a rare occurrence), the most likely culprit is a member of the Candida genus. In terms of C. parapsilosis and arthritis, most cases have occurred after either arthrocentesis (removal of excess fluids from the joints of either the knee, ankle, elbow, or hip) or implantations of prostheses.2
Otomycosis
Otomycosis is the result of an infection in the ear causing inflammation of either the middle or outer ear.2 The risk factors for developing otomycosis caused by C. parapsilosis, includes trauma to the ear and previous antimicrobial treatments.2
Onychomycosis
Onychomycosis is an infection of the nail (finger or toe) that is caused by various microorganisms—including fungi.2
This is one of the ‘diseases’ that can be contracted outside of the hospital. Adults are usually the ones that suffer the most from this disease, and it occurs when there has been an injury to the nail and then exposure to C. parapsilosis (through activities such as gardening).2
It is the second most common ‘cause’ of onychomycosis after the dermatophyte Trichophyton rubrum.5
Vulvovaginitis
Vulvovaginitis is the inflammation of the vagina and the vulva due to the presence (and overgrowth) of Candida species. In terms of the number of women who will experience vulvovaginitis—it’s stated that 70 to 75% of women will experience at least one episode during their reproductive years.4
C. parapsilosis is one of the three non-Candida albicans species that can cause vulvovaginitis.2
Treatment for Candida parapsilosis infections
The best treatments for C. parapsilosis infections rely on the proper diagnosis and identification of the fungi/yeast by medical professionals. While there are antifungal and antimicrobial treatments available, if improperly prescribed or used, these can lead to reoccurring infections or the pathogen becoming resistant to treatments.2 Depending on where the C. parapsilosis infection has occurred, surgery to physically remove the fungi may also be required, as C. parapsilosis is slowly becoming more resistant to various antimicrobial treatments.2
C. parapsilosis and the microbiome
C. parapsilosis, is a normal inhabitant of the microbiome and unless presented with an opportunity for invasion, it does not typically cause any problems.
References:
- Ciurea CN, Kosovski IB, Mare AD, Toma F, Pintea-Simon IA, and Man A. (2020) “Candida and Candidiasis—Opportunism versus Pathogencity: A Review of the Virulence Traits” Microorganisms 8:857; doi:10.3390/microorganisms8060857
- Trofa D, Gácser A, and Nosanchuk JD. (2008) “Candida parapsilosis, an Emerging Fungal Pathogen” Clinical Microbiology Reviews 21(4): 606-625
- Mamtani SS, Aljanabi NM, Gupta Rauniyar RP, Acharya A, and Malik BH. (2020). “Candida Endocarditis: A Review of the pathogenesis, morphology, risk factors, and management of an emerging and serious condition” Cureus 12(1): e6695. DOI 10.7759/cureus.6695
- Makanjuola O, Bongomin F, and Fayemiwo SA. (2018) “An Update on the Roles of Non-albicans Candida species in Vulvovaginitis” Journal of Fungi 4(121): doi:10.3390/jof4040121
- Kukhar Y, Smagulova A, Daniyarova A, Baiduissenova A, and Kiyan V. (2020) “Candida parapsilosis as a Causative Agent of Onychomycosis in Patient with Cirrhosis of the Liver” Journal of Fungi 6(313): doi:10.3390/jof6040313
- Image by nadya_il from Pixabay