With an estimated global prevalence of 240 million people, Osteoarthritis (OA) is the most common form of arthritis.1 As a degenerative joint disease, OA can lead to decreased mobility, quality of life, pain, and loss of productivity.1,2 It is also associated with a heavy societal burden concerning social expenditure and an increased reliance on healthcare services.1,2
Individualized osteoarthritis therapeutics
The available therapeutic options for osteoarthritis are currently limited. Emerging research indicates that new treatments should account for disease heterogeneity (variability).1 There are multiple phenotypes (characteristics, properties, developmental pathways, and mechanisms) of arthritis.1
These phenotypes include the bone phenotype and the inflammatory phenotype.1 Designing different therapeutic approaches that are tailored to each phenotype may lead to improved treatment responses for those living with OA.1
Osteoarthritis bone phenotype
Characterization of the bone phenotype includes bone marrow lesions that appear deep within the bone.1 These lesions can be observed through magnetic resonance imaging (MRI) and are generally indicative of osteoarthritis.1
Bisphosphonates are disease-modifying OA drugs that are usually ineffective for this phenotype of osteoarthritis.1 Research on knee OA suggests that zoledronic acid infusions or strontium ranelate may be better options for reduced pain perception, bone marrow lesion size, and cartilage volume loss.1
Osteoarthritis inflammatory phenotype
Synovium is a connective tissue that lines joint capsules which can become inflamed. Inflammation of the synovium (synovitis) is a common characteristic of the inflammatory phenotype of OA.1,3 The inflammatory phenotype is observed in hand osteoarthritis and can be detected using MRI and ultrasound.1
Some anti-inflammatory agents used to treat rheumatic diseases may be effective for treating the symptoms of those with the inflammatory phenotype.1 Etanercept, an inhibitor of the inflammatory cytokine tumour necrosis factor (TNF), improves patients’ perception of pain and induces joint remodelling.1 However, not all TNF inhibitors available show the same positive effects in reducing pain.1
Detecting osteoarthritis phenotypes
In addition to using imaging technologies to detect osteoarthritis phenotypes, blood and urinary analysis of biochemical markers may also serve as effective tools.1 For example, concentrations of inflammatory cytokines like C-reactive protein can help assess inflammation.1 Similarly, collagen type I, II, or III levels can provide information on bone and cartilage turnover.1
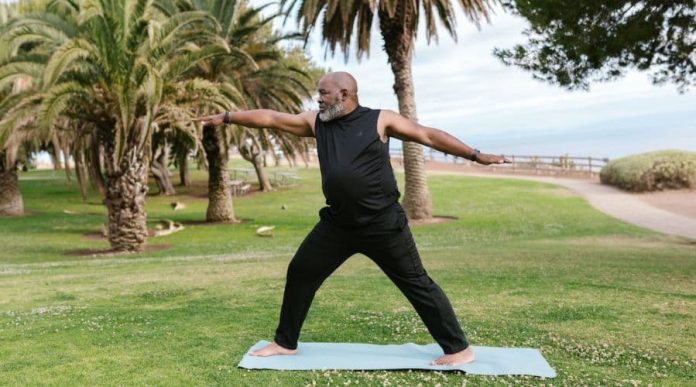
Improving osteoarthritis symptoms with regular physical activity
Research suggests that regular physical activity may help improve symptoms associated with osteoarthritis. It was found that exercise can improve pain, mobility, and quality of life for those living with OA, specifically of the knees or hips.2
The findings have significant implications for knee osteoarthritis in elderly patients. Those aged 65 years or older have the highest risk for loss of independence compared to any other medical condition impacting this demographic.2
Results from the review indicate that participating in moderate-intensity exercise for a minimum of 45 minutes per week may lead to health improvements.2 However, while recreational activities improved physical function, only aerobic and resistance exercises reduced pain in people with knee and hip OA.2
Overview
New research in the field of osteoarthritis demonstrates that disease phenotypes should be prioritized in designing new therapeutics.1 While addressing phenotypes may help develop new clinical trials for OA treatments, patients can take action immediately to improve symptoms and enhance their quality of life by regularly exercising. Please consult your healthcare provider to learn more about osteoarthritis and its management.
References
- Van Spil WE, Kubassova O, Boesen M, Bay-Jensen AC, Mobasheri A. Osteoarthritis phenotypes and novel therapeutic targets. Biochem Pharmacol. 2019;165:41-48.
- Kraus VB, Sprow K, Powell KE, Buchner D, Bloodgoods B, Piercy K, George SM, Krausi WE. Effects of physical activity in knee and hip osteoarthritis: A systematic umbrella review. ACSM. 2019;51(6):1324-1339.
- Van den Bosch MHJ. Osteoarthritis year in review 2020: biology. Osteoarthr Cartil. 2021;29(2):143-150.
The article below contains sponsored links to other sites; these links are being provided as a convenience and for informational purposes. The editorial staff of the Medical News Bulletin had no role in the preparation of the contents of these linked sites and are not responsible for the accuracy or content of the linked sites. The views and opinions expressed in the sponsored links are those of the advertiser and do not reflect those of the Medical News Bulletin. The Medical News Bulletin does not accept liability for any loss or damages caused by the use of any products or services, nor do we endorse any products, services, or links in our sponsored links.